The Madras High Court’s ruling mandates IRDAI to accord the same status to AYUSH treatments as allopathic treatments in the matter of medical insurance reimbursement.
Case Title: K Krishna and Another v The Managing Director and Others
Case No: W.P.(MD)Nos.18130 & 18131 of 2021
Decided on: 21st November, 2023
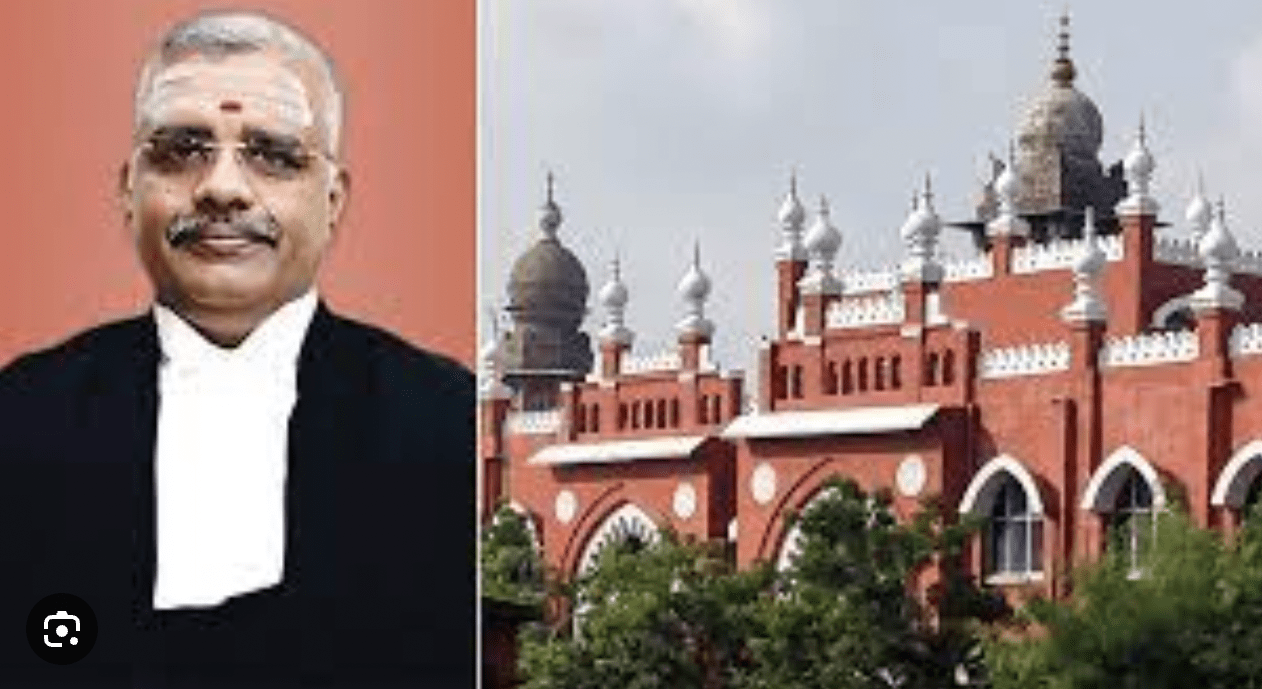
CORAM: HON’BLE MR. JUSTICE N. ANAND VENKATESH
Introduction
The Madras High Court while hearing a plea for full reimbursement of costs incurred for treatment under AYUSH ruled mandating the IRDAI to accord the same status to AYUSH treatments as allopathic treatments in the matter of medical insurance reimbursement.
Facts of the Case
In the present case, two petitioners owned insurance policies with M/s. Star Health and Allied Insurance Company. An advocate and an advocate clerk, the petitioners, each obtained policies in 2009 for amounts of Rs. 5 lakhs and Rs. 4 lakhs, respectively. The petitioners requested compensation for medical expenses of a sum of Rs.52,25 each paid during treatment for COVID-19 at Siddha Hospital.
The insurance company paid back only Rs. 15,000 to the first petitioner and Rs. 10,000 to the second, claiming that the upper limits for reimbursement towards treatment taken in AYUSH Hospital is fixed at Rs.15,000 for the policy of sum of Rs.5 lakhs and fixed at Rs.10,000 for the policy of Rs.4 lakhs established by the norms of the Insurance Regulatory and Development Authority of India (IRDAI). The petitioners contend that there was no distinct cap for AYUSH (Ayurveda, Yoga) when they took the policy in 2009.
As per the policy in 2009, the costs related to medical care provided under non-allopathic medical systems would not be covered and they are not obligated to pay for any costs associated with treatment under AYUSH. With the approval and license of the Insurance Regulatory and Development Authority of India (IRDAI).
Courts analysis and decision
The court observed that there was broader concern in hand and traditional medicine was advised for those who were affected during the COVID-19. Notably, patients had significant relief from AYUSH therapies. Limiting the reimbursement cap under these conditions is irrational because it would prevent policyholders from getting paid for costs, they incurred in AYUSH hospitals. It is imperative that the Insurance Regulatory and Development Authority of India (IRDAI) acknowledge patient’s entitlement to select their treatment of choice, whether it be allopathic or conventional AYUSH techniques. Treating the costs of both types of treatment equally is crucial since it would be unfair to favour allopathy over AYUSH. It is imperative that allopathic medicines be given the same weight as traditional AYUSH treatments in India.
The court further held that according to the policies submitted, the insurance company has already complied with its duty by paying the petitioners the maximum amount allowed by the policy. As a result, there is no justification for giving the insurance company further instructions to pay the petitioner’s entire claim sum.
“PRIME LEGAL is a full-service law firm that has won a National Award and has more than 20 years of experience in an array of sectors and practice areas. Prime legal fall into a category of best law firm, best lawyer, best family lawyer, best divorce lawyer, best divorce law firm, best criminal lawyer, best criminal law firm, best consumer lawyer, best civil lawyer.”
Written by- Rupika Goundla